Samantha Spellicy
On Her Personal Everest and Summiting the Terrain of the Brain
By: Cynthia Adams | Photos By: Nancy Evelyn
When Samantha Spellicy took the stage during the 3MT® competition at Ciné, a theater in Athens, she gave a straight talk about stroke research and the high incidence of strokes occurring in the “Stroke Belt.” The sobering facts were that if you lived (or were born) in the geographic region you were potentially twice as likely to suffer a stroke.
Silence fell.
Everyone had no doubt heard of the Bible Belt. But the audience learned that Athens is smack in the midst of another defining phenomenon. The state of Georgia joins several southern states in the so-called “buckle” of the Stroke Belt.
Such a distinction is an attention getter. Even for a young, presumably healthy audience like her contemporaries, the message Spellicy delivered resonated. “Living in Georgia, I’m sure you’ve all seen a hose or a sprinkler watering a lawn on a hot summer’s day,” her three-minute talk began. “Now imagine if that hose became clogged or blocked. You could see how the grass on the other side of the clog, wouldn’t be able to get the water or nutrients it needs. Over time the grass would begin to whither and eventually die.” With only three minutes for her full message, she moved swiftly:
“This is exactly what happens in a type of stroke called ischemic stroke, where a blood vessel of the brain becomes clogged or blocked and the brain tissue on the other side of the blockage can’t get the nutrients it needs such as oxygen and glucose from the blood. Over time, this brain tissue begins to die, and we see this death as the physical manifestations of stroke, such as difficulty with walking or controlling limbs, facial paralysis, and speech impairments.”
When the votes were tallied, Spellicy had netted one of three prizes, winning the People’s Choice 3MT® award.
As for the rate of strokes occurring within a 10-state area, Spellicy later discussed what created the belt’s terrifying parameters. The “stroke belt” nomenclature breaks down into a number of predictors.
“Diet; exercise; comorbidity; what keeps coming back is one individual thing is not the full answer. It’s the combination.”
Athens, with a population of roughly 127,000, may be a small town, but consider this:
“Based upon the South’s average numbers, each person in Athens knows someone who has had a stroke,” Spellicy said.
The health care industry is well aware of the probability of a high stroke incidence even in smaller urban areas. “St. Mary’s Hospital can do interventional radiology. Two good hospitals for stroke are right here.”
There are only three hospitals in all of Georgia offering stroke victims interventional radiology. Athens has two of them. One of them, Piedmont Athens Regional Medical Center, won an award last July from the American Heart Association for its interventional program and efficacy.

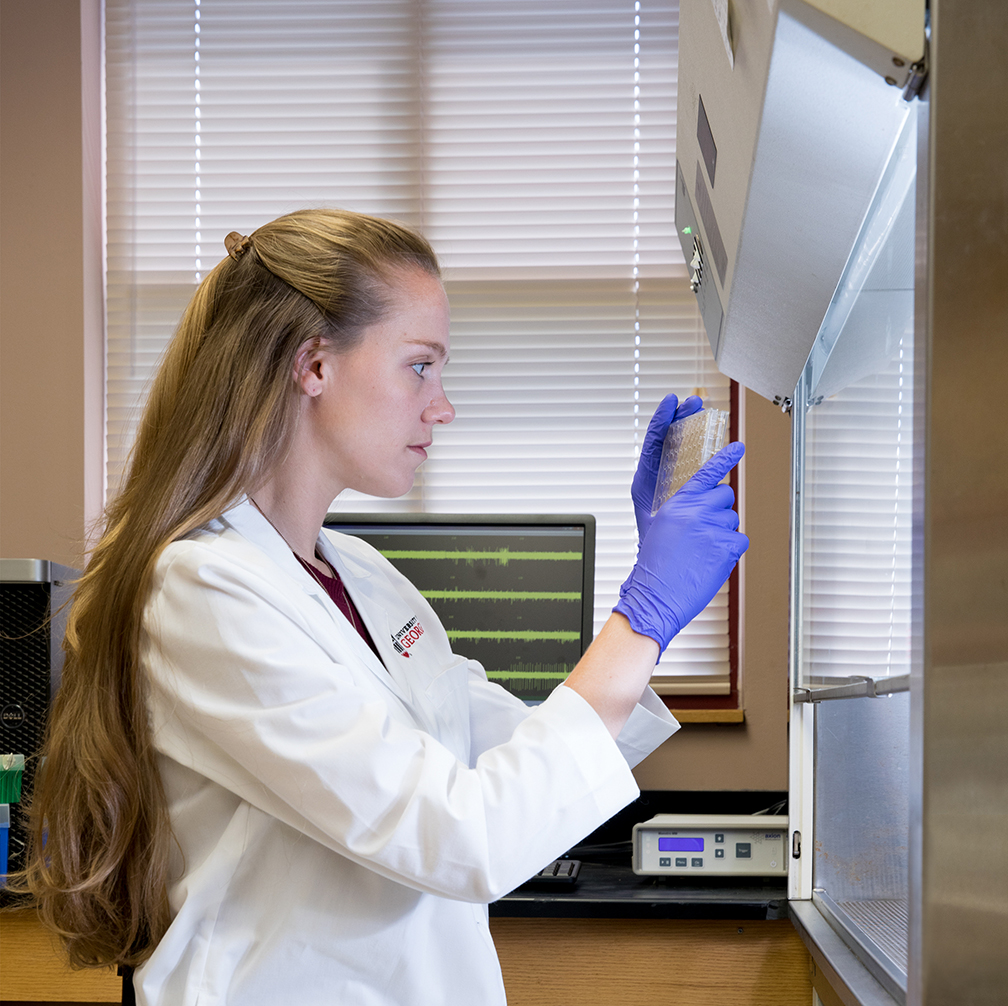
University of Georgia’s Samantha Spellicy is earning combined doctoral and medical degrees. She works in Steven Stice’s lab at the Rhodes Center for Animal and Dairy Science. What they are learning might change everything for the future of the Stroke Belt. What does Spellicy know that we should also know?
When you look at a map of stroke incidence and look Southward, “it’s like a heat wave here,” notes the young researcher. Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Virginia, and Tennessee, comprise the infamous region of the Stroke Belt.
Spellicy was born outside the belt, but her interest in stroke research is spurred by a fascination with the brain.
“The brain is the last frontier of medicine,” she explains. “Everything else has been fleshed out.”
She adds, “It’s like the Everest of medicine.”
 The Stroke Belt is an 11-state region of the United States where studies show that the risk of stroke is 34 percent higher for the general population than it is in other areas of the country. It spans across the South, with rates particularly high in the region. States in the Stroke Belt include Mississippi, Tennessee, Louisiana, Kentucky, Georgia, North Carolina, Alabama, South Carolina, Arkansas, Indiana and Virginia. In Mississippi, the stroke risk is one third higher than the national average. Deaths from stroke are much more common for people of all ages and the overall rate of cardiovascular disease is higher than the national average. Researchers believe that greater than- average rates of obesity, cigarette smoking and high blood pressure account for the increased risk of death from cardiovascular disease in the Stroke Belt. thepreventioncenter.com
The Stroke Belt is an 11-state region of the United States where studies show that the risk of stroke is 34 percent higher for the general population than it is in other areas of the country. It spans across the South, with rates particularly high in the region. States in the Stroke Belt include Mississippi, Tennessee, Louisiana, Kentucky, Georgia, North Carolina, Alabama, South Carolina, Arkansas, Indiana and Virginia. In Mississippi, the stroke risk is one third higher than the national average. Deaths from stroke are much more common for people of all ages and the overall rate of cardiovascular disease is higher than the national average. Researchers believe that greater than- average rates of obesity, cigarette smoking and high blood pressure account for the increased risk of death from cardiovascular disease in the Stroke Belt. thepreventioncenter.com
At 29 years old, Spellicy has completed six of the eight years required to earn combined doctoral and medical degrees. She finished two years of medical school at the Medical College of Georgia in Augusta, and four years of her doctoral research in neuroscience at UGA. She will earn her PhD in neuroscience this year.
At UGA, she is a student researcher in the Regenerative Bioscience Center, where she assists professors Steven Stice and Franklin West, who are working with neural stem cell derived therapeutics.
Spellicy’s a compelling speaker, as proven by her 3MT® win, and also a great proponent for a dual degree program. “There are great things about both,” she says.
The idea of doing both was spurred by a natural curiosity and desire to be both involved with patients and also conduct research. Prior to her own pursuit, she had never met anyone else pursuing both a PhD and M.D. Nor did she have a family member who had opted to do either.
“I didn’t know anyone (in doctoral studies) who was pre-med,” Spellicy says. In truth, she didn’t even have a close acquaintance doing pre-med studies either, and while her parents were professionals, neither were researchers nor physicians.
“I just knew I wanted to do both.” Actually, Spellicy’s love of science and research developed fairly recently. Previously, she was following a different path. While an undergraduate at the University of Maryland studying journalism, government and politics, she found herself repeatedly signing up for science elective courses.
“One day, an advisor said, ‘Why don’t you become a science major?’”
Spellicy says the suggestion changed her academic direction. She did an about-face.
“I’d never thought of it. It sounded like a good idea. I’d always liked the brain, and Maryland had a physiology and neurobiology major.”
She shifted to a new academic track, which required her to scramble to make up for science credits.
Spellicy is nearing the final segment of her studies at the Medical College of Georgia, where she will complete her M.D. in 2022. When she returns to Augusta next year, she will begin medical rotations through different specialties.
She already knows what course she will likely take. “I’m leaning towards neurology. Maybe neurosurgery.”
Possibly, says the young woman who enjoys children, she will choose pediatric neurosurgery.
Despite the relative rarity of a dual degree, Spellicy scoffs at the idea that she possesses unusual talent Nope, she says. She attributes it more to tenacity. Seizing the moment.
“I wouldn’t say anyone’s more talented than anyone else. It’s just opportunity.” She pauses. I’m about to go to the lab and work another six hours. I’d say it’s about the effort.”
Disparate things have contributed to Spellicy’s interest in becoming a pediatric neurosurgeon in the near future.
She admits she has physical aptitude, which would place her in good stead, and knows how to check her squeamishness when witnessing surgeries. Also, she laughs, a fondness for gaming has taught her to be nimble.
“I play a lot of video games. I have good dexterity.” In American medical schools, women are being accepted at a higher rate than men (source: the Association of American Medical Colleges).
The combination of practicing physician and clinical researcher can be attributed to her following several interests that weren’t exclusive. Spellicy completed her undergraduate degree at Maryland in neuroscience, then began post baccalaureate study in infectious diseases at the National Institutes of Health. While at NIH, she heard the chief of Neurology deliver a memorable lecture about opportunities in research.
“I enjoyed it,” she recalls. It was a lecture that would again change her trajectory. She mentions a pivotal moment when the neurologist mentioned important stroke research at UGA.
It caught her attention.
Afterward, Spellicy investigated doctoral studies at UGA, soon learning that the combination M.D./PhD program was unique.
Was Spellicy the kid that always had a great science project? She laughs and shakes her head “no.”
Except.
Actually, there was a second-grade presentation she put together on the subject of stars and their lifespan. She was asked to present to other, higher grades. Then Spellicy modestly changes the subject, saying, “I think it starts then. As a kid.” She strongly believes kids should be exposed to science and will benefit, adding from childhood she was a typical sponge, soaking up knowledge, a child with infinite curiosity.
“I loved it all.”
“If I got in trouble, I couldn’t watch educational television,” she says, laughing heartily. (“My parents must have laughed!” she adds.) “I remember being in 2nd grade. Watching ‘The Magic School Bus’,” she recalls fondly. “It was my bread and butter.”
From that child absorbed by basic scientific principles, Spellicy has progressed to tackling one of the most challenging academic tracks.
Her current work with stroke research is looking at something that halts the further deterioration of brain tissue following a stroke, and even regeneration.
“The whole key is not to only halt the damage, but use a therapeutic to regenerate.”
There are numerous metrics they consider, Spellicy explains, in establishing a predictive model that can be used with patients. They consider the lesion size after imaging the brain with MRI.
“Currently, after someone has a stroke, the doctor has to guess. We don’t have anything concrete we can tell you.” Spellicy examines data in trying to make a predictive model in order to tell stroke patients “how bad their gait is going to be and what kind of an improvement they can expect.”
Spellicy says the pig model created here in the Rhodes Center at UGA “may have been the first in the U.S.” They are specifically accumulating knowledge on
how to repair and regenerate brain tissue following stroke.
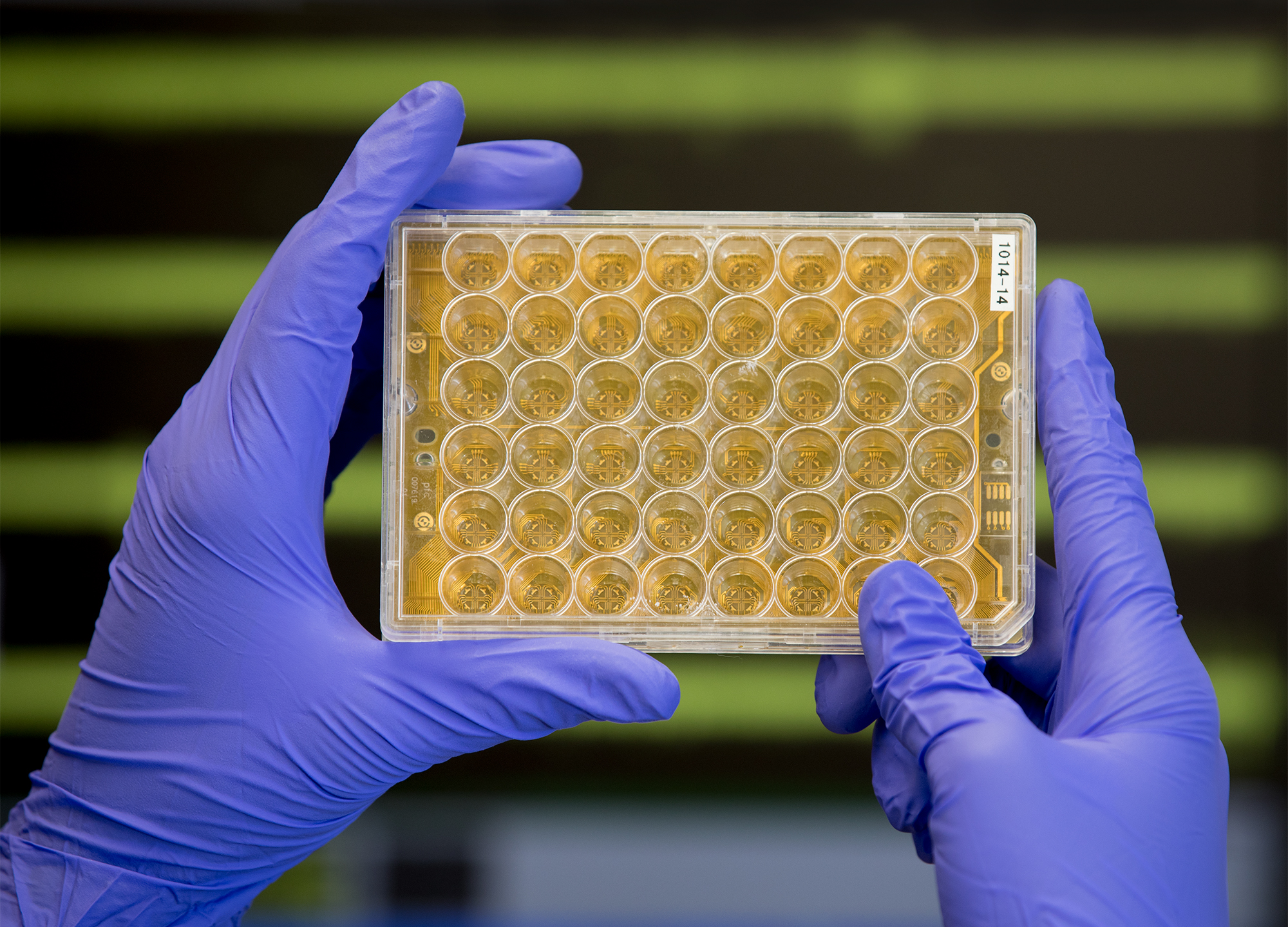
“This is a Multi-Electrode Array (MEA) 24-well plate, built to work with a special MEA system that allows us to read the electrical activity of cells that are plated into each of those wells,” explains Spellicy. “We can use those plates to mimic certain diseases or conditions (for example, inflammatory activation), then measure the electrical activity and see how it changes the culture. Then we can test a new therapeutic or a drug, by adding to the culture and seeing if we can reverse or prevent a change in the electrical activity to begin with.”
What would her dream job look like? “It’s going to differ a lot. A balance of both clinical and research.” She says she would definitely seek patient interaction during her work week, combined with lab time. “I wouldn’t just want to do solely one or the other.”
Here in the stroke belt, Spellicy is hyper-aware of health matters.
It matters little that her vantage point is that of a young researcher, one at a fit age with a healthy and informed perspective. She knows whereof she speaks.
She notices the Southern proclivity for salty, fried foods and sweetened drinks. Her grandmother will call her and “ask if she can eat bacon,” she laughs. As for prevention, Spellicy says, “I think everyone should have some kind of nutrition education…it’s not even in our schools today.”
Are things changing for the better in the stroke buckle? Ostensibly. Maybe.
“A few years ago, Fitbits were huge,” she muses. “I don’t know if the motivation of having a Fitbit is the biggest change. Perhaps it’s awareness. The biggest change is people being aware.”
Spellicy emphasizes what we’ve heard before: that exercising even 30 minutes a day, perhaps only twice a week, can decrease your cardiovascular risk.
“I have to trick myself into exercising,” she laughingly admits.
However, she swims, goes to the gym, and plays a lot of sports. Spellicy is an avid volleyball and softball player, and even plays in the Athens softball league. Running, however, is not her thing.
There is also the matter of her own experience of brain surgery. A few years ago, when Spellicy was two months into her medical studies in Augusta, she was struck by a car while walking.
This landed her in the hospital with injuries that required surgeries to both her shoulder and brain. The experience will definitely make her a better doctor, she notes. The emotional and physical toll continue to remind her of the ordeal.
“I just got new front teeth,” she says, smiling widely, pleased that the new crowns are completely natural looking.
The scar, where a metal plate was inserted in her shoulder, is visible but she shrugs this off, too.
Spellicy ventures to consider the future, one where strokes may hold less frightening, less catastrophic and less morbid consequences.
“Something that seems pretty awful might not be in five more years.”
In her own words: the following is Spellicy’s summary of what her clinical work with the stice lab signifies.
“A BIG DRIVING FORCE in stroke right now is to develop better predictive models of expected outcome for stroke patients. After the first initial hours of a stroke, and after a patient has been stabilized and has transitioned to road to recovery, the next thing most patients and patients’ families want to know is what that road looks like, how long it will take, and what is their hope to regain motor control, cognitive function and speech (depending on where the stroke is located). Additionally, with other diagnoses such as a heart attack, there are ‘biomarkers’ such as a troponin blood tests, that doctors can discretely measure and say, ‘Yes this value is high so most likely you are having a heart attack that is of x level of severity.’
“In stroke, however, they don’t really have a good one or anything you can test and measure that easily or that are reliable. There are some indicators and factors doctors can use to he p assess and inform patients on all these questions, but there is always room for improvement to really develop more concrete models that can help predict level of functional recovery or initial stroke severity.
 “Therefore, I was attempting to use MRI measurements as a way to develop these predictive models and really come up with a single , noninvasive parameter which physicians could use to say based on this assessment I predict your road to recovery will look like x.
“Therefore, I was attempting to use MRI measurements as a way to develop these predictive models and really come up with a single , noninvasive parameter which physicians could use to say based on this assessment I predict your road to recovery will look like x.
“To do this I worked with the West lab at UGA (and my own lab, the Stice lab) in the regenerative bioscience center (RBC) to measure over 15 parameters in various MRI sequences of pigs that had a stroke 24 hours prior. We then worked together to measure the pigs’ gait (walking down a track -taking over 65 measurements such as cadence, velocity, step length, etc.) and behavior in an ope n field. Then, I created a correlation matrix of the MRI measurements to the 90 measurements of functional outcomes (gait and behavior) to see which things were significantly correlated for each pig at each time point.
From all of this work and analysis I was able to find one measurement, that was significantly predictive of functional outcomes at acute (24 hours) and chronic (84 days) time points.
“This neuroimaging measurement is really easy for physicians to do not only on MRI, but also on CT, and even with ultrasound (a couple papers showing this), which means it would be easily adaptable for physicians to use and most already know how to make this measurement which is also a plus. Based on the data I acquired from these pig stroke studies, it looks promising that this could be a useful measurement for predicting human patient outcomes after stroke.”
As for the pig brain model, Spellicy adds why it is more appealing than some other animal models of stroke: “So that model was really new and initiated by the West lab here at UGA. The pig was chosen because their brain is a lot closer to a humans than more common rodent models not only structurally (amount of white to gray matter and organization), but also in size (which is important to test therapeutic doses), and in complexity (gyrencephallly vs. rodents which have lissencephaly—just means pigs have those waves and wrinkles in their brains whereas rodent brains are smooth and don’t really have the same surface area).”